you’re not alone!
Healthcare is a complicated field with many moving parts, and two essential components that often go unnoticed by the average person are credentialing and contracting.
These processes play a pivotal role!
They ensure that healthcare providers can deliver quality care while maintaining a financially stable practice.
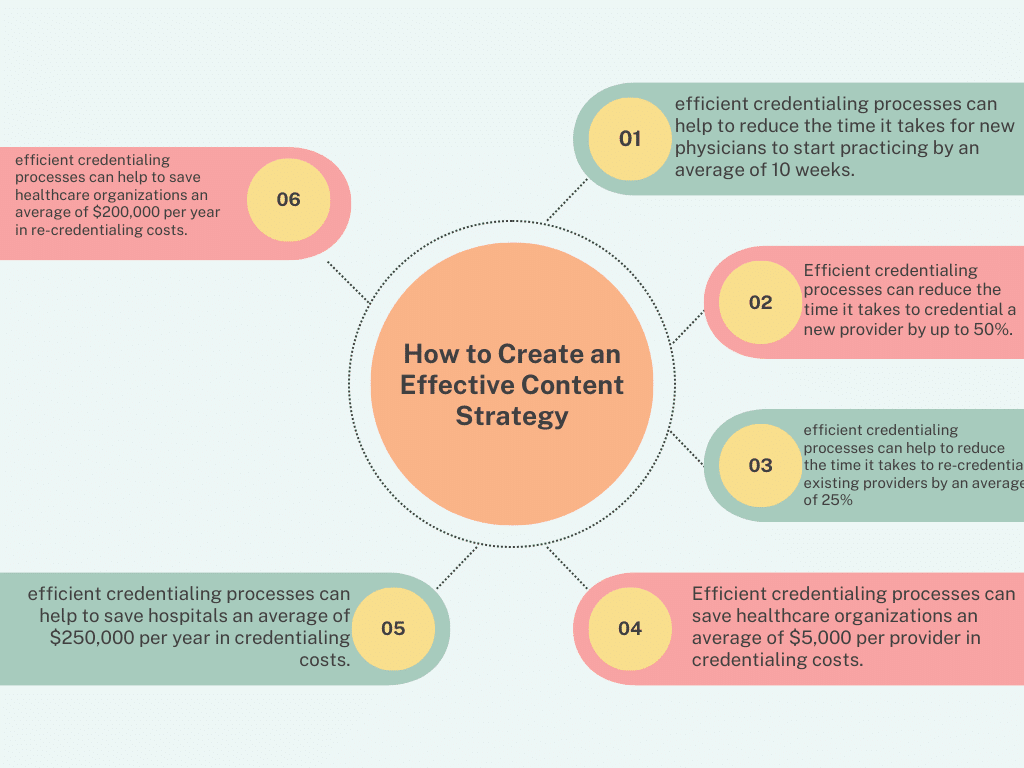
Current data on the time and cost savings associated with efficient credentialing processes
Time Savings
- Efficient credentialing processes can reduce the time it takes to credential a new provider by up to 50%. This can save healthcare organizations an average of 30 days per provider.
- A study by the American Medical Association found that efficient credentialing processes can help to reduce the time it takes for new physicians to start practicing by an average of 10 weeks. This can save hospitals an average of $25,000 per physician.
- A study by the Healthcare Financial Management Association found that efficient credentialing processes can help to reduce the time it takes to re-credential existing providers by an average of 25%. This can save healthcare organizations an average of 15 days per provider.
Cost Savings
- Efficient credentialing processes can save healthcare organizations an average of $5,000 per provider in credentialing costs.
- A study by the American Medical Association found that efficient credentialing processes can help to save hospitals an average of $250,000 per year in credentialing costs.
- A study by the Healthcare Financial Management Association found that efficient credentialing processes can help to save healthcare organizations an average of $200,000 per year in re-credentialing costs.
In this article, I am going with you in the world of healthcare credentialing and contracting, demystifying their importance and explaining how they work.
Understanding Credentialing in Healthcare
Credentialing in healthcare is the process by which healthcare organizations, insurance companies, and government agencies verify and validate the qualifications and professional backgrounds of healthcare providers.
It process ensures that those who provide medical services are qualified, competent, and meet the standards required to deliver safe and effective care.
Key Steps in Credentialing
Application Submission: Healthcare providers, including physicians, nurses, and other allied health professionals, must submit detailed applications. These applications include educational history, training, licensure, certifications, and work experience.
Primary Source Verification: Credentialing organizations verify the information provided by healthcare providers by directly contacting the institutions, licensing boards, and organizations responsible for the provider’s credentials.
Peer Review: Many credentialing bodies employ a peer review process, where a committee of experienced healthcare professionals evaluates the applicant’s qualifications and clinical competence.
Credentialing Decision: After thorough verification and review, a decision is made regarding the provider’s eligibility to join a healthcare network or work within an organization.
Re-credentialing: Credentialing is not a one-time event. Healthcare providers are periodically re-credentialed to ensure they maintain their qualifications and adhere to professional standards.
The Significance of Credentialing
Credentialing serves several critical purposes in the healthcare industry:
Patient Safety: It ensures that patients receive care from qualified professionals, reducing the risk of medical errors and improving overall patient safety.
Insurance Reimbursement: Credentialing is often a prerequisite for healthcare providers to be reimbursed by insurance companies, which is crucial for maintaining financial stability.
Legal Compliance: Credentialing helps healthcare organizations comply with state and federal regulations, protecting them from legal issues related to unqualified staff.
The World of Contracting in Healthcare
Have you ever heard that contracting in healthcare involves the negotiation and establishment of agreements between healthcare providers and insurance companies, government agencies, or healthcare organizations?
These contracts outline the terms and conditions under which healthcare services will be provided and reimbursed.
Key Components of Healthcare Contracts
Fee Schedules: Contracts specify the fees or reimbursement rates that healthcare providers will receive for specific services. These rates can vary depending on factors such as location and the provider’s specialty.
Network Participation: Healthcare providers agree to be part of a specific network, which can affect their patient base and the number of patients referred to them.
Quality Metrics: Some contracts include performance metrics that providers must meet to maintain their contract status. These metrics often focus on quality of care and patient outcomes.
Claims and Payment Processes: Contracts detail the process for submitting claims and receiving payments, including the timeline for reimbursement.
Termination Clauses: Contracts may include provisions for termination, outlining the conditions under which either party can end the agreement.
The Significance of Contracting
Contracting is essential for healthcare providers for several reasons:
Revenue Stream: Contracts provide a stable revenue stream for healthcare providers by specifying how and when they will be paid for their services.
Patient Access: Contracting with insurance companies or healthcare organizations can expand a provider’s patient base, increasing their access to potential clients.
Legal Protections: Contracts provide legal protections for both parties, ensuring that the terms of the agreement are upheld and preventing disputes.
The Synergy Between Credentialing and Contracting
Credentialing and contracting are closely interconnected in the healthcare industry. Here’s how they work together:
Credentialing as a Prerequisite: Before entering into contracts, healthcare providers often need to complete the credentialing process to demonstrate their qualifications and eligibility to participate in healthcare networks.
Contract Negotiations: Once credentialed, healthcare providers can negotiate contracts with insurance companies or healthcare organizations. Credentialing assures payers that they are dealing with qualified providers.
Compliance and Performance: To maintain contract status, providers must adhere to credentialing requirements, ensuring they remain qualified and competent.
Patient Trust: Credentialing and contracting together build patient trust. Patients have confidence in providers who are part of their insurance network and who have undergone a thorough credentialing process.
Conclusion
So I hope you have learned everything you need to know about the role of credentialing and contracting. Credentialing verifies the qualifications of healthcare professionals, while contracting establishes the terms under which services are provided and reimbursed.
Simplify Billing Services is your gateway to achieving operational excellence in healthcare. Our array of services is designed to meet the diverse needs of healthcare providers.
Embark on your journey to improvement by exploring our services:
- Accounts Receivable Management Services: Enhance your revenue flow by clicking here.
- Revenue Cycle Management Services: Optimize your financial performance with us here.
- Credentialing and Contracting Solutions: Ensure your practice is properly credentialed with payers. Learn more here.
- Eligibility and Benefits Verification Solutions: Simplify your verification process by visiting us here.
- Medical Billing and Coding Services: Streamline your billing and coding processes. Discover how we can assist you here.
Simplify your healthcare operations with Simplify Billing Services. Start your journey towards success today!