In the intricate realm of healthcare, managing revenue efficiently is paramount. At the heart of revenue cycle management (RCM) lies the crucial process of prior authorization. Whether you’re a beginner or an advanced professional in the healthcare industry, this comprehensive guide will equip you with the knowledge and strategies needed to navigate and excel in the world of prior authorization.
The Significance of Prior Authorization
Prior authorization is the process by which healthcare providers obtain approval from a patient’s insurance provider before certain medical procedures, treatments, or services can be administered. This step is essential because it ensures that the treatment is medically necessary and covered by the patient’s insurance plan.
About the Author
Before we delve into the intricacies of prior authorization, it’s important to establish credibility. I am James Roger and I bring 3 years of experience in the healthcare industry with a specialized focus on revenue cycle management and prior authorization processes. Over the years, I have earned relevant certifications and affiliations to establish my authority on this topic.
Understanding Prior Authorization
What is Prior Authorization?
Prior authorization is a critical process in healthcare revenue cycle management that requires obtaining approval from a patient’s insurance provider before specific medical procedures, treatments, or services can be rendered. This process verifies the medical necessity and insurance coverage for the services.
Why is Prior Authorization Necessary?
Prior authorization serves several essential purposes:
- Cost Control: It helps prevent unnecessary medical expenses by confirming that a specific treatment or service is warranted.
- Patient Care: Ensures that patients receive the most appropriate and effective care.
- Revenue Management: Contributes to a smoother revenue cycle by reducing denials and delays.
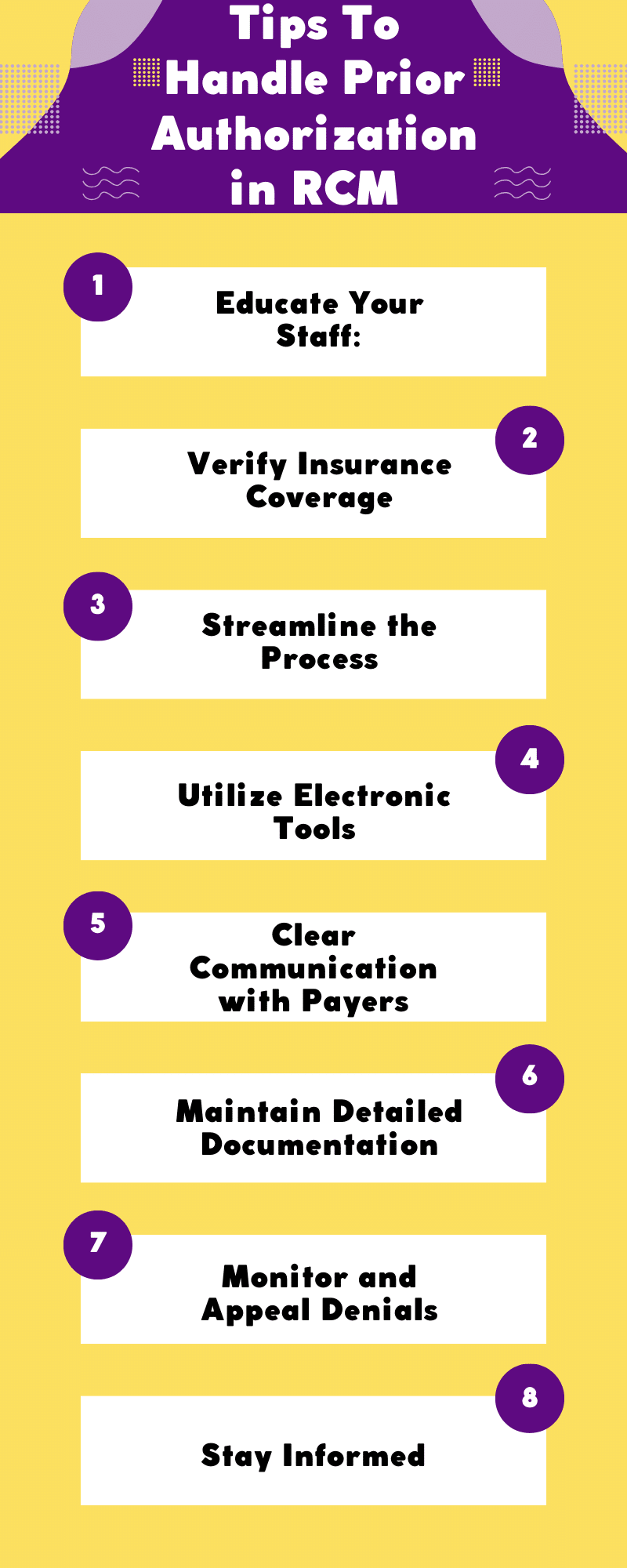
Tips To Handle Prior Authorization in RCM
Handling prior authorization in revenue cycle management (RCM) can be a complex and time-consuming process, but it’s essential for ensuring timely reimbursement for medical services. Here are eight tips to help you effectively manage prior authorizations in RCM:
Educate Your Staff:
Ensure that your billing and administrative staff are well-trained and up-to-date on the latest prior authorization requirements, codes, and procedures. Regular training sessions can help them stay informed about changes in regulations and insurance policies.
Verify Insurance Coverage:
Before providing any non-emergency medical services, verify the patient’s insurance coverage and review the specific requirements for prior authorization. This step helps prevent denials and delays in reimbursement.
Streamline the Process:
Implement efficient workflows and technology solutions to streamline the prior authorization process. This may include using electronic health record (EHR) systems, practice management software, and automated authorization request tools.
Utilize Electronic Tools:
Leverage electronic prior authorization solutions offered by payers whenever possible. These tools can reduce the paperwork and administrative burden associated with manual authorization requests.
Clear Communication with Payers:
Establish open lines of communication with insurance companies. Develop relationships with payer representatives or dedicated points of contact who can assist in navigating the authorization process. Ask for clear guidelines and written confirmation of authorization when necessary.
Maintain Detailed Documentation:
Accurate and detailed documentation is crucial throughout the prior authorization process. Keep comprehensive records of all communications, including authorization request forms, letters, faxes, and emails. Ensure that patient records also reflect the authorization status.
Monitor and Appeal Denials:
Continuously monitor the status of authorization requests and promptly address any denials. Understand the reasons for denial and be prepared to appeal if necessary. Having a well-documented appeals process can help secure authorizations and reimbursements.
Stay Informed:
Keep up to date with changes in insurance policies, medical codes, and regulatory requirements. This includes regularly checking for updates from payers and attending seminars or webinars related to prior authorization best practices.
The Challenges of Prior Authorization
Navigating the prior authorization process can be fraught with challenges. Understanding these common pain points is essential for mastering the process.
Administrative Overhead:
Prior authorization often involves a significant administrative burden, diverting valuable time and resources from patient care.
Denials and Delays:
Frequent denials or delays in the prior authorization process can disrupt patient care, impact revenue flow, and lead to patient dissatisfaction.
Regulatory Complexities:
The ever-evolving regulatory landscape can make navigating the prior authorization process perplexing. Staying updated is essential for compliance.
Prior Authorization Workflow
A successful prior authorization process follows a well-structured workflow. Here’s a simplified breakdown:
Verification of Insurance Coverage:
Early verification of a patient’s insurance coverage and the specific requirements for prior authorization is crucial to avoid delays and denials.
Gathering Patient Information:
Collect all necessary patient information, including medical history and diagnosis codes, to support the authorization request.
Communication with Payers:
Efficient communication with payers is essential for clarifying requirements, addressing issues, and ensuring the smooth flow of the authorization process.
Submission and Tracking:
Submit authorization requests through the appropriate channels and diligently track the progress of each request.
Authorization Status Checks:
Regularly check the status of authorization requests to ensure timely responses and address any issues promptly.
Beginner’s Guide: Building a Solid Foundation
For those new to the world of prior authorization, here are some fundamental strategies to build a strong foundation.
Automating the Process:
Consider adopting RCM software that automates the prior authorization process. Automation reduces administrative overhead and minimizes the risk of errors.
Staff Training:
Ensure that your staff is well-versed in the latest guidelines and regulations for prior authorization. Regular training sessions are invaluable for keeping your team updated.
Documentation and Record-keeping:
Maintain meticulous records of prior authorization requests, approvals, and communications. Well-organized documentation simplifies audits and appeals.
Eligibility Checks:
Implement a system that checks a patient’s eligibility and coverage in real-time, allowing you to identify issues before they cause delays.
Intermediate Techniques: Enhancing Efficiency
For those with some prior experience, these intermediate techniques will help enhance efficiency and effectiveness.
Electronic Prior Authorization (ePA):
Adopt ePA tools to facilitate electronic communication with insurance providers, streamlining the authorization process and reducing manual paperwork.
Monitoring Key Metrics:
Consistently monitor metrics related to prior authorization, such as approval rates, denial reasons, and turnaround times, to identify areas for improvement.
Streamlining Communication:
Establish efficient communication channels with payers. Regular communication helps clarify requirements and resolve issues promptly.
Utilizing Clinical Decision Support:
Use clinical decision support tools to align treatment choices with insurance coverage and medical necessity, reducing denials and ensuring proper care.
Advanced Strategies: Streamlining and Optimizing
For seasoned professionals and organizations, advanced strategies are essential to streamline and optimize prior authorization.
Centralizing Authorization Workflow:
Create a centralized workflow for handling prior authorizations. This promotes consistency, accountability, and efficient utilization of resources.
Predictive Analytics:
Leverage predictive analytics to anticipate authorization needs and optimize resource allocation.
Data Integration and Reporting:
Integrate data from electronic health records (EHR) and other systems with your RCM for more comprehensive reporting and improved decision-making.
Compliance and Regulations
Understanding and navigating the regulatory landscape is essential when dealing with prior authorization.
Navigating the Regulatory Landscape:
Stay up-to-date with federal and state regulations, as well as payer-specific guidelines, to ensure compliance in the prior authorization process.
Key Compliance Strategies:
Implement key compliance strategies, including ensuring proper documentation, adhering to privacy and security standards, and conducting regular audits.
Addressing Privacy and Security:
Prior authorization often involves the exchange of sensitive patient information. Addressing privacy and security is crucial to comply with regulations such as HIPAA.
Technology and Tools
Technology plays a pivotal role in streamlining prior authorization processes. Explore some of the key tools and solutions.
Software Solutions for RCM:
Consider adopting robust RCM software that offers features specific to prior authorization, making the process more efficient and reliable.
Artificial Intelligence in Prior Authorization:
Artificial intelligence (AI) can assist in automating routine tasks, verifying patient information, and even predicting authorization outcomes.
Integrating EHR and RCM Systems:
Integration of EHR and RCM systems allows for seamless data sharing, reducing the need for manual data entry and ensuring data accuracy.
FAQs (Frequently Asked Questions) Prior Authorization in RCM
What medical services typically require prior authorization?
Common services requiring prior authorization include surgeries, certain diagnostic tests, specialized medications, and durable medical equipment. The exact list varies by insurance plan.
How long does the prior authorization process typically take?
The duration can vary significantly. Simple cases may take a few days, while complex cases could take weeks. It’s crucial to start the process early to avoid delays in patient care.
Can prior authorizations be appealed if denied?
Yes, prior authorizations can be appealed. The process typically involves providing additional documentation and justifications for the requested service.
How do electronic prior authorizations (ePA) work?
ePA systems facilitate electronic communication between healthcare providers and insurance companies. They streamline the prior authorization process by reducing paperwork and allowing for faster responses.
What are the privacy and security concerns in prior authorization?
Privacy concerns include the protection of patient health information during the process. Security concerns encompass the secure exchange of information between healthcare providers and payers.
What are the advantages of using predictive analytics in prior authorization?
Predictive analytics can help forecast the volume of prior authorizations, allocate resources efficiently, and predict potential denials, allowing organizations to proactively address issues.
How can I stay updated with changing regulations in prior authorization?
Regularly check government healthcare websites, subscribe to industry publications, and attend relevant conferences or webinars. Many organizations also offer compliance training.
Conclusion
In conclusion, mastering the art of prior authorization is vital for an efficient revenue cycle management process. By implementing the strategies outlined in this guide, you can improve the accuracy, efficiency, and compliance of your prior authorization processes. It’s time to take action and optimize your RCM for better patient care and financial stability.